
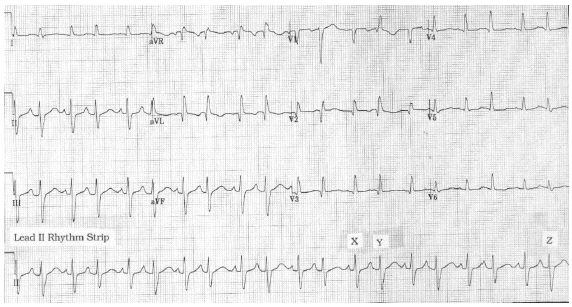
Zipes MD, in Clinical Arrhythmology and Electrophysiology (Third Edition), 2019 Junctional RhythmĪn accelerated junctional rhythm typically develops within a few seconds of RF delivery at the effective ablation site ( Fig. The treatment is sedation, paralysis, cooling, and intravenous amiodarone. JET is associated with marked tachycardia (>180 beats/min), important hemodynamic compromise, and increased mortality rates. JET occurs almost exclusively in neonates or young children undergoing major congenital cardiac surgery. If treatment is necessary, an intravenous β blocker is appropriate.Ī malignant variation of accelerated junctional rhythm is junctional ectopic tachycardia (JET). Accelerated junctional rhythm is virtually always a transient phenomenon in the setting of heightened adrenergic tone. The mechanism of accelerated junctional rhythm is either enhanced or abnormal automaticity, and pacing or cardioversion cannot terminate it. Occasionally, the atrial ECG demonstrates AV dissociation, in which case irregular cannon waves are seen instead. Depending on the ventriculoatrial interval, regular cannon A waves may be visible on the central venous pressure (CVP) trace (see Chapter 8). Retrograde-conducted P waves that follow the QRS are visible on an atrial ECG and may be seen on a standard rhythm strip ( Fig. The tachycardia typically develops gradually (warm up), slowly increasing up to a heart rate of 110 to 150 beats per minute. Warren Smith, Margaret Hood, in Cardiothoracic Critical Care, 2007 Accelerated Junctional RhythmĪccelerated junctional rhythm (nodal tachycardia) is a regular narrow-complex tachycardia in which no P wave can be seen preceding the QRS complex. For chronic symptomatic junctional rhythm not associated with sinus node dysfunction, ablation of the junctional focus may be considered but with risk of creating AV block ( Table 3.6). Permanent pacemaker implantation can alleviate symptomatic junctional rhythm associated with sinus node dysfunction. Discontinuation of medications that may slow the sinus rate may allow the atrial rate to increase and override a slower junctional rhythm (“capture”). Treatment of the junctional rhythm is usually not necessary, but treatment of the underlying problem (e.g., underlying sinus or atrial bradycardia) may be needed. These symptoms (which can be vague and easily missed) include lightheadedness, palpitations, effort intolerance, chest heaviness, neck tightness or pounding, shortness of breath, and weakness. Junctional rhythm can cause symptoms due to bradycardia and/or loss of AV synchrony. Junctional rhythm usually is associated with a benign course, but it can cause symptoms due to AV dyssynchrony (pseudo “pacemaker syndrome”). It can also be seen as part of tachy-brady syndrome. It can be caused by necessary medications (e.g., β-adrenergic blockers, verapamil, digitalis, sotalol, amiodarone).

Junctional rhythm can be due to hypokalemia, MI (usually inferior), cardiac surgery, digitalis toxicity (rare today), sinus node dysfunction, or after ablation for AV node reentrant tachycardia. Because the atrial and QRS rhythms are independent, AV dissociation will be present capture beats will document the absence of AV block as the cause of the AV dissociation. 3.15), with its usual rate of 40 to 60 bpm being exceeded, particularly with adrenergic stimuli. Junctional rhythm can be an accelerated rhythm ( Fig. Holter monitoring may be useful to document the presence of sinus node dysfunction and the cause of any symptoms that might result from the rhythm. The junctional rate is usually 40 to 60 bpm. P waves may be absent, or retrograde P waves (inverted in leads II, III, and aVF) either precede the QRS with a PR of less than 0.12 seconds or follow the QRS complex. Junctional rhythm is a regular narrow QRS complex rhythm unless bundle branch block (BBB) is present. Nora Goldschlager MD, in Arrhythmia Essentials (Second Edition), 2017 Junctional rhythm Description Atrial fibrillation: Symptoms and causes /diseases-conditions/atrial-fibrillation/symptoms-causes/dxc-20164936 Acute management of atrial fibrillation: Part I.

Atrial fibrillation /medicalpubs/diseasemanagement/cardiology/atrial-fibrillation/ (2017, February 6) /HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/Atrial-Fibrillation-Medications_UCM_423781_Article.jsp (2015, August 13) cdc.gov/dhdsp/data_statistics/fact_sheets/fs_atrial_fibrillation.htm You can learn more about how we ensure our content is accurate and current by reading our editorial policy. Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.


 0 kommentar(er)
0 kommentar(er)
